A first in PH spine surgery
Ligaya Aglipay, a 68-year-old retiree from Isabela, had lost hope. Since December 2022, she had suffered from unbearable pain in her posterior and left leg. Tests revealed a stage 4 metastatic tumor on her sacrum, the triangular bone at the center of the pelvis. Several doctors had recommended palliative care, a medical approach for terminal illness.
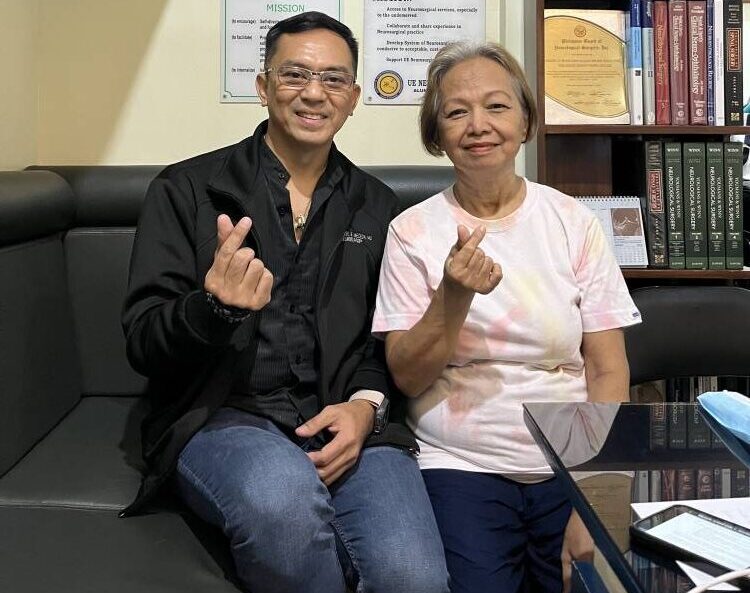
In early August, Aglipay and her family found hope. Neurosurgeon Dr. Elmer Jose Meceda performed the country’s first—and only the world’s second—minimally invasive removal of a tumor at the base of the spine at the University of the East Ramon Magsaysay Medical Center (UERMMMC). The day after her surgery, Aglipay felt immediate relief from the pain.
The procedure, endoscopic spinal surgery (ESS), uses tiny incisions and slender instruments guided by a special camera to visualize and treat the affected area. Endoscopy is a procedure that examines the structures of the body at close range. This minimally invasive approach significantly reduces tissue damage, blood loss and postoperative pain, leading to faster recovery.
In the past, surgeons operated on common cases such as disc stenosis (narrowing of the spinal canal) and compression. “Now, we have started operating on tumors in the spine using the endoscope,” says Dr. Meceda. “Previously, we would only remove a section of the tumor. Now, the tumor can be completely excised. This is a significant advancement for endoscopy.”
In 2019, UERMMMC made history when Dr. Meceda performed the country’s first ESS on the neck in one hour. At the height of the pandemic in 2021, he accomplished the world’s first endoscopic slip disc surgery done through the mouth at the Bicol Medical Center.
Managing cancer
When Aglipay was diagnosed with cancer, she was given morphine to manage the severe pain. A biopsy revealed that the cancer was a distant metastasis, having spread from the primary organ, the thyroid, to the outlying sacrum.
“The patient didn’t feel any pain from the thyroid,” says Dr. Meceda. “The first thing diagnosed was the tumor in the sacrum. Results from the biopsy indicated papillary thyroid cancer.”
Aglipay underwent a thyroidectomy, complete removal of the thyroid gland, in November 2023, followed by radioactive iodine ablation (RAI), a treatment for thyroid cancer. RAI targets and destroys cancer cells. When administered orally, the body absorbs the radioactive iodine, which is then concentrated in the thyroid gland and any thyroid cancer cells, even those that have spread. This localized radiation eliminates the cancerous tissue.
Early this year, Aglipay was still enduring severe pain. She had consulted other doctors who recommended palliative care.
“For a patient, it’s like accepting that you’re at the end of the line,” recalls Dr. Meceda. “Palliative care is more focused on pain management rather than primary care. The family was desperate.”
The MRI results revealed that the tumor on the sacrum was compressing the nerves. “Initially, I was planning to decompress the nerve roots by removing the top part of the tumor,” says Dr. Meceda. “This is called debulking, where you remove 50 percent of the tumor and then do another round of RAI.”
Dr. Meceda had never performed ESS for tumor removal in the sacrum before, but he believed he could accomplish it. For two weeks, he consulted his foreign mentors and visualized the procedure and the successful outcome.
“I would be dreaming of the procedure,” says Dr. Meceda. “Before I operate on my patients—particularly for procedures that have never been done before—I go through the motions 20 to 30 times in my mind before the actual practice.”
Hope
Aglipay underwent the procedure on a Friday. “The next day, she sat up and felt no pain,” says Dr. Meceda. “I told the nurses to stop the pain medications. By Sunday, she was fit to be discharged.”
Asked by family members about the future of their mother’s health, Dr. Meceda explained that papillary thyroid cancer is a common type and has the best outlook for patients in terms of longer survival rates.
Dr. Meceda cites the advantages of ESS: “There is minor injury to the skin and muscles. Because healing is faster, there is less hospital cost. If patients need additional treatment, they can have it sooner. No need to wait for weeks or months. The primary benefit is that the patient can rest and move around more quickly.”
He adds, “It’s been a month since post operation. The patient reports that there is minimal pain and she is back to her daily routine in household work.
“Her family had nearly lost hope until recently. I told them that if ESS didn’t work, I would have to perform open surgery. In the past, we would only get a sample of the tissue for biopsy to determine the cancer. Now, we can perform a total incision. I want to highlight that the Philippines is not behind the world in terms of medical advancements.”

















