My uterus was a drama queen—I finally showed her the door
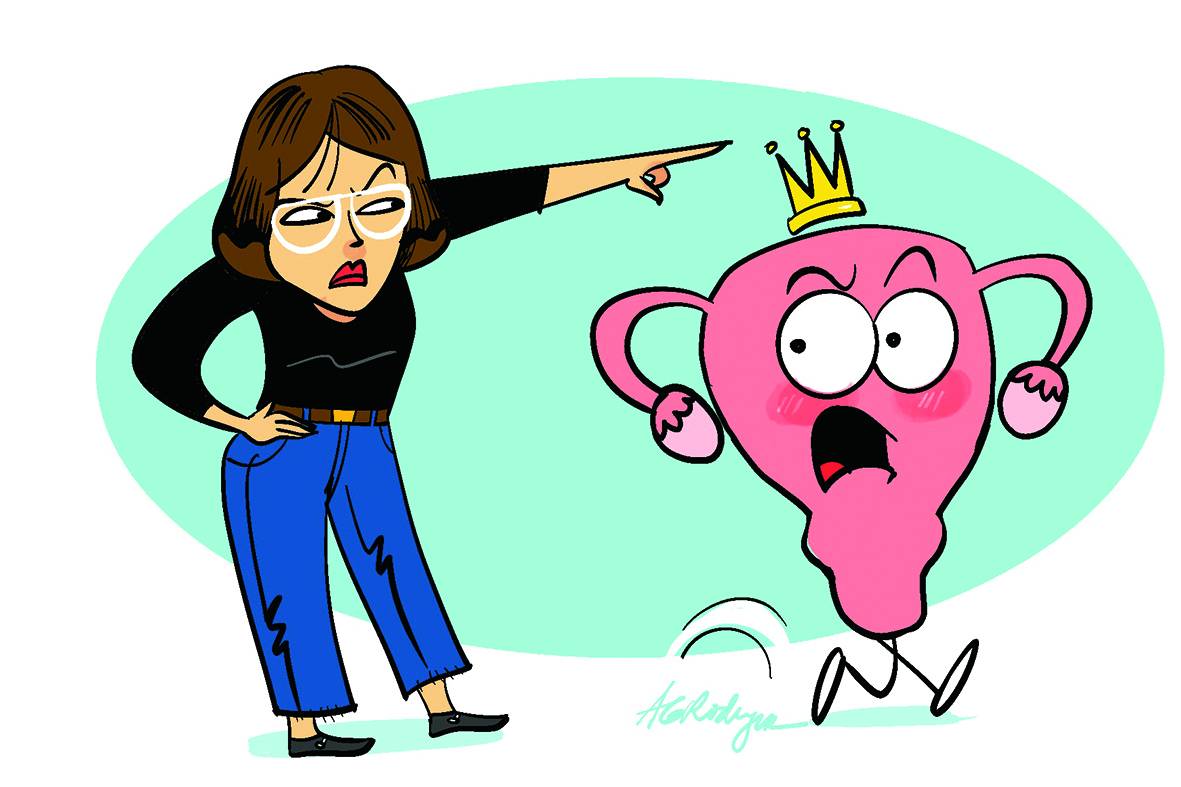
My uterus and I had a toxic relationship. She was high-maintenance, unpredictable, and made every month feel like a medieval punishment. Cramps? Check. Bloody mess? You bet. A flair for drama that rivaled a soap opera villain? Oh, absolutely.
At first, I thought we could work it out—maybe with some heating pads, a good dose of ibuprofen, and the occasional desperate prayer to the goddess of pelvic peace. But no. She had other plans.
My uterus wasn’t content with cramps and a polite monthly visit. No—she was staging a full-blown massacre every few weeks, at a surprising regularity. I’m talking super-heavy bleeding that made splatter film directors look lazy. Endless doses of tranexamic acid didn’t help.
So when my good and kindly gynecological oncologist, Dr. Jay Arnold Famador at Makati Medical Center, gently suggested it might be time to part ways with the dang uterus, I was surprised at myself for hesitating a little. Okay, maybe not just a little—it took me almost a full year to say yes.
“If it’s just the inconvenience, I can live with it,” I reasoned, not thrilled at the prospect of being butchered on the table, though in the back of my head, I was hoping against hope that menopause would come sooner instead, please oh please!
“But your case isn’t that simple. I don’t want to miss anything,” Doc Jay cautioned. “We can’t just keep doing a D&C.”
A D&C (dilation and curettage) is a procedure used to remove endometrial polyps from the lining of the uterus for both treatment and biopsy to rule out cancer or other abnormalities.
I understood clearly, but like many a woman in an abusive relationship, I wasn’t quite ready for a clean break.
Breast cancer survivor
For context, I’m a seven-year breast cancer survivor. In early 2018, as part of my treatment, I was prescribed the anticancer medicine tamoxifen, which I have to take for 10 years or until menopause, whichever comes first.
The thing about tamoxifen is that, while it may keep the recurrence of breast cancer at bay, it can also increase the risk of endometrial or uterine cancer.
During hospitalization last year, where I was treated for iron deficiency anemia, likely caused by the monthly heavy bleeding, an ultrasound showed that I had endometrial polyps. These are growths on the inner lining of the uterus that are usually benign, but could be a red light for someone on tamoxifen. An eventual biopsy showed the polyps to be benign.
Another ultrasound months later, however, showed that there were polyps again. Doc Jay reminded me that there’s not much that can be done at that point, and, again, that he can’t keep doing a D&C. I finally relented.
The treatment plan was to perform a total abdominal hysterectomy with bilateral salpingo-oophorectomy (TAH-BSO), which is a strategic and sometimes preventive decision.
A TAH-BSO is often performed on former breast cancer patients—especially those with hormone receptor-positive cancers (I was HER2-negative)—to reduce estrogen production, which can fuel cancer growth. Removing the uterus, ovaries, and fallopian tubes lowers the risk of gynecologic cancers and eliminates hormonal stimulation that could lead to recurrence. It may also be done as a preventive measure in patients with BRCA gene mutations (the kind Angelina Jolie has).
Endometrial polyps are a relatively common gynecological condition, with prevalence depending on factors like age and clinical symptoms. A large-scale Danish study, for instance, found a 7.8 percent overall prevalence, with increasing rates in postmenopausal women—up to 11.8 percent. In women presenting with abnormal uterine bleeding, the prevalence of endometrial polyps can rise to 25 percent.
TAH-BSO is also a common gynecologic surgery, especially in women at elevated risk for ovarian or uterine cancers (e.g., BRCA mutation carriers). In the United States, approximately 600,000 hysterectomies are performed annually, and among women undergoing this surgery, 40 to 78 percent also have their ovaries and fallopian tubes removed, depending on their age group.
Specifically, bilateral oophorectomy (removal of both ovaries) is performed in 40 percent of women ages 40–44, 60 percent ages 45–49, and 78 percent ages 50–54, often as a preventive strategy against estrogen-driven cancer recurrence.
Gap in research
Despite the relatively high prevalence of endometrial polyps and the frequency with which procedures like TAH-BSO are performed, there’s a notable gap in research dedicated to less invasive, targeted treatments—especially in patients with comorbidities like breast cancer. Most clinical pathways still rely heavily on radical surgical intervention, often preemptively, due to limited understanding of the natural history, recurrence risk, and malignant potential of polyps in high-risk populations.
This reflects a broader issue in gynecologic care: insufficient investment in long-term, conservative management strategies backed by high-quality longitudinal studies.
This is not just a theoretical concern. Several of my closest friends have also undergone hysterectomies, highlighting just how routine this surgery has become, even for benign conditions. In countries like the Philippines, abdominal hysterectomy remains significantly more common than laparoscopic or minimally invasive techniques used in more advanced health-care systems. This matters: Abdominal surgery typically involves longer recovery times (6-8 weeks vs 1-2 weeks for laparoscopy), higher risk of complications like infection and bleeding, and greater overall physical and emotional impact.
The continued reliance on major surgery underscores the urgent need for more research, better screening tools, and more conservative, evidence-based treatment pathways for managing gynecologic conditions—especially in settings where surgical technology and access to preventive care remain limited.
So yes, the uterus is often treated like a suspicious package—removed “just to be safe.” And while science has taken us to the moon and back, we’re somehow still relying on 20th-century methods to deal with polyps.
Until then, we’ll continue cheering each other through recovery with soup, heating pads, and shared war stories—because if there’s one thing women excel at, it’s healing from major surgery like it’s just another item on the to-do list.