The silent threat of that tingling feeling

Many of us are familiar with that tingly sensation we get on our palms in cold weather. Or that rush of pins and needles in our legs and feet that makes us stagger ever so slightly when we abruptly stand up after sitting in an awkward position.
Usually, we dismiss them as random natural body phenomena. And that’s what they are most of the time. But what if these sensations happen, persist, or worsen with no apparent reason?
You may have developed a condition called peripheral neuropathy (PN), a nerve disease that impairs sensation and movement, and whose symptoms include numbness, prickling, and stabbing or burning pain—mostly in the hands or feet.
And if you’re a diabetic, it may be prudent to pay your doctor a visit.
According to medical experts in an online talk hosted by P&G Health, there are some 537 million people with diabetes globally—4.3 million of them Filipinos. And 2021 statistics show that one in two diabetics and one in 10 prediabetics (those with impaired glucose tolerance but whose levels have yet to reach or breach diabetes thresholds) suffer from PN.
While diabetes is the leading cause of PN, there are other factors that contribute to the disease, such as alcohol misuse and B vitamins deficiency.
But because PN’s symptoms often start off mildly, and are usually perceived as negligible or chalked up to aging, most patients who have it don’t realize they already have it until it has already progressed. In fact, eight out 10 patients remain undiagnosed.
“Many people affected by this disease are not aware that their symptoms are due to PN, because it often develops slowly, almost silently, over long periods of time,” said Dr. Rizaldy Pinzon, a neurologist at the Bethesda Hospital in Indonesia.
Lack of awareness
Making diagnosis even trickier is that there’s a tendency in some physicians or healthcare professionals to “deprioritize” PN over other conditions when assessing diabetics.
“Barriers among patients and the community include lack of awareness of PN and risk factors, not noticing early signs, not seeing a doctor on time, and difficulties verbalizing the symptoms. Physicians, on the other hand, often struggle with crowded clinics and limited time, lack of awareness and routine to diagnose PN,” said Dr. Francis Pasaporte, consultant for diabetology at Iloilo Provincial Hospital.
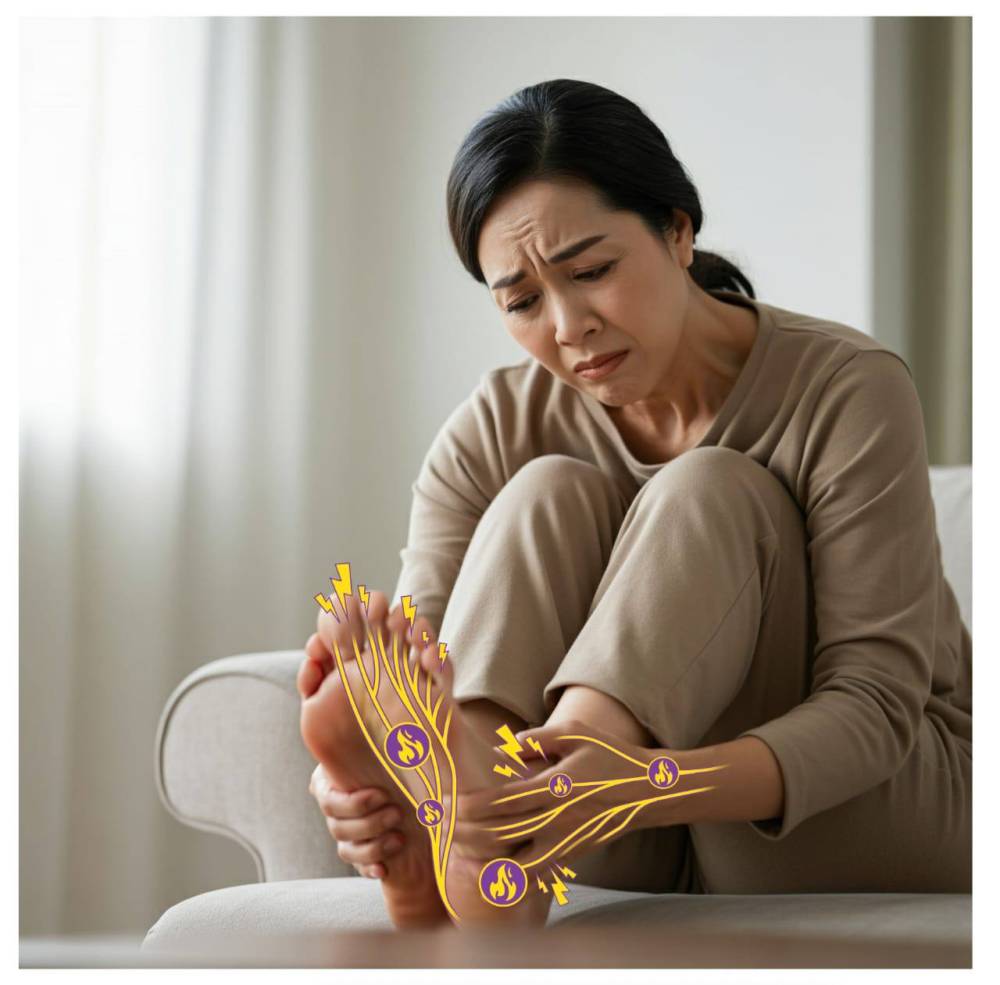
Left untreated, PN’s manifestations could eventually go from frustrating to aggravating to downright debilitating. Damage to the nerves can make the simplest task, like buttoning a shirt or squeezing a tube of toothpaste, a chore. Holding a bottle can be painful. Daily activities, in short, become a challenge.
“Suddenly, the patients start losing mobility. They have difficulty walking stairs or driving … They struggle executing simple day-to-day activities like cooking. They have difficulty sleeping, or get injuries in their feet that they don’t notice—all due to the progressing nerve damage,” Pinzon added.
Ankle reflexes dwindle and temperature perception goes haywire, increasing the risk of accidents, especially among the elderly. PN can also increase a diabetic’s risk of developing foot ulcers, which, at worst, could lead to amputation.
Horror stories
There are also instances in which patients develop “negative symptoms,” which means they become so numb they’re unable to feel anything at all.
“There are horror stories that we have seen or heard of people walking around with nails or thumbtacks on their feet without them even knowing it,” said Dr. Bien Matawaran, consultant for endocrinology, diabetes and metabolism at the University of Santo Tomas Hospital.
But things don’t have to reach that point. Nerve damage, doctors stressed, can be reversed if recognized early. And to help address the issue, P&B Health—in collaboration with international experts from different fields like neurology, dermatology, and pharmacy—has devised a simple online diagnostic test that can facilitate early PN diagnosis.
Called the Neurometer Pro, the tool is a self-screening questionnaire that will help users understand if their nerve health is at risk for PN. After answering only five questions (pertaining to kind and location of symptoms, time of flare-ups, impact on quality of life, and other health risk factors), the test gives out a score in the end approximating the user’s risk.
The results can then be presented to a doctor for assessment. “This reduces screening time for physicians, and empowers patients to act early to avoid long-term complications,” Aditya Gupta, P&G Health senior marketing director for Asia Pacific, said of the Neurometer Pro, which is available for free in the Philippines, Indonesia and Malaysia. (Visit pgamaphc.jebbit.com.)
Early detection
While it may not always lead to cure, “knowledge,” doctors said, can help “heal.” Pharmacist and university professor Dr. Kenny Merin is a testament to this philosophy.
In the six months leading to his diabetes diagnosis in 2023, Merin started to feel a constant urge to urinate—one of the most common early signs of the disease.
But there was more: He noticed subtle, prickling sensations in his limbs. Before he knew it, the tingling had progressed into bouts of pain that could only be likened to “electric shocks.” Sometimes, it was as if he had put on some invisible gloves, affecting the way he gripped objects.
There was also weakness in his hands and feet that often worsened at night, making it hard for him to go to sleep. And this confluence of aggravations, he said, made everyday life not only physically draining, but also mentally taxing.
Merin, assistant vice president for academics and research at the Lyceum of the Philippines-Davao, knew that his symptoms were consistent with PN. And because he has a history of diabetes in his family, he deduced that he may already be suffering from both disorders.
A series of laboratory tests eventually confirmed his hunch.
But thanks to his knowledge, coupled with ample doses of vigilance and foresight, early detection was done, allowing Merin to act swiftly and accordingly.
Merin is, of course, a medical professional, and therefore better equipped to identify his symptoms as PN. But with new and accessible diagnostic tools, and continuous efforts by health groups and patient communities to drive awareness about PN, more people could very well catch the disease before it starts compromising their quality of life.
“By helping people understand signs and symptoms in a relatable manner, and the role of early diagnoses and timely treatment, we can empower them to take proactive steps toward seeking treatment and improving their quality of life,” Merin said.