Study: Depression among PH youth doubles in 8 years

The number of Filipino youth experiencing depression has more than doubled in just eight years, with some of the most vulnerable sectors in this age group being disproportionately affected.
This was one of the key findings of a new study conducted by a Filipino research team and published by Cambridge University Press.
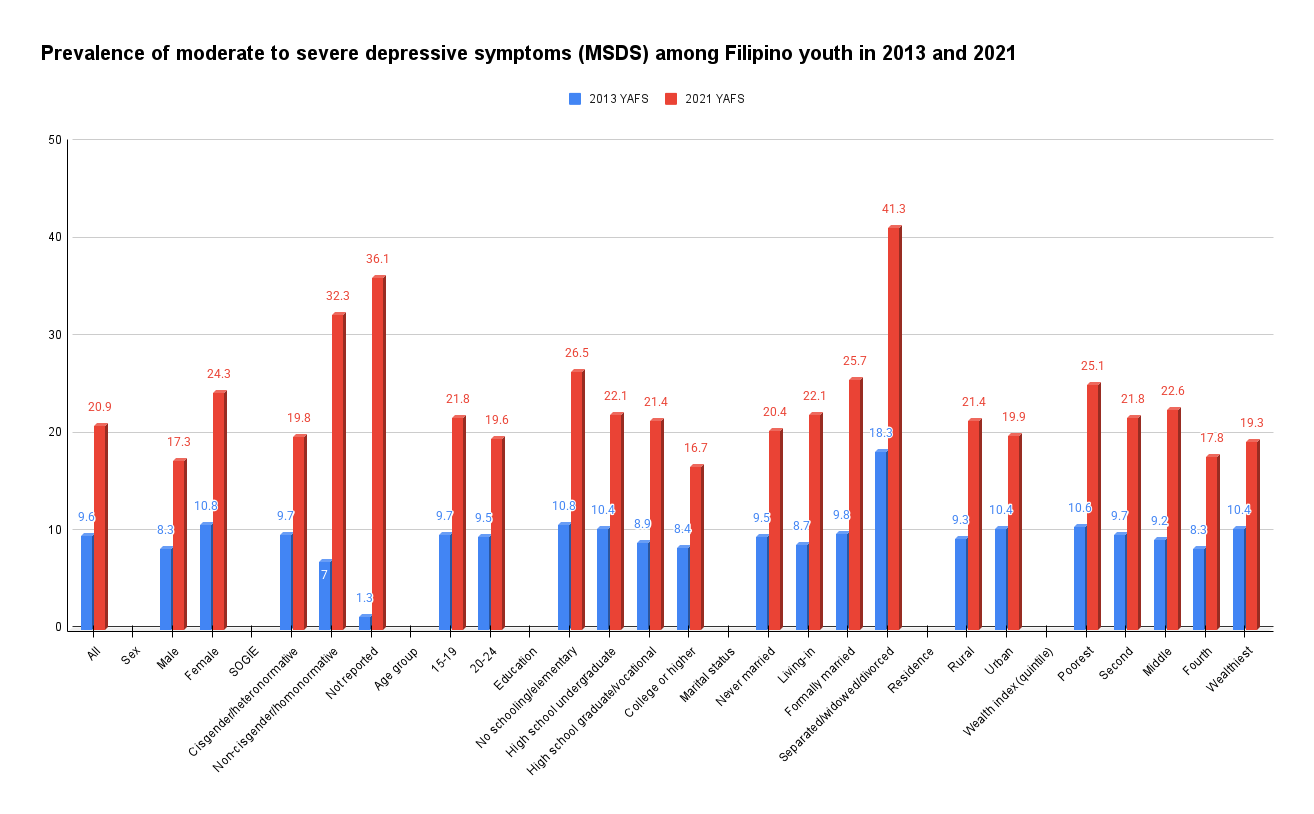
The researchers found that the prevalence of moderate to severe depressive symptoms (MSDS) among Filipinos age 15 to 24 years old rose from 9.6 percent percent in 2013 to 20.9 percent in 2021, highlighting a significant decline in youth mental health.
While COVID-19 contributed to the notable increase in the prevalence and sociodemographic disparities in MSDS, it was also deemed likely that depression among Filipino youth was already on the rise before the pandemic.
“This increase not only underscores the deteriorating mental health landscape for young people in the Philippines but also signals a potential crisis that could have long-term implications for individuals and society as a whole,” the study said.
Sample data
The peer-reviewed study, “Rising prevalence of depression and widening sociodemographic disparities in depressive symptoms among Filipino youth: findings from two large nationwide cross-sectional surveys,” was published in Cambridge Prisms: Global Mental Health of the Cambridge University Press in April.
The all-Filipino research group is composed of Joseph Puyat of the Centre for Advancing Health Outcomes and the University of British Columbia in Canada; Divine Salvador and Anna Tuazon of the University of the Philippines (UP) Diliman; and Sanny Afable of the University of St. Andrews in the United Kingdom. (Tuazon also writes a column in the Inquirer that comes out Thursdays.)
They analyzed data from the 2021 and 2013 survey rounds of the Young Adult Fertility and Sexuality Study (YAFS), a nationwide probability survey of Filipino youth age 15 to 24 conducted mainly by the UP Population Institute.
The 2013 YAFS was conducted among 19,178 Filipino youth across the country, while the 2021 YAFS had a sample size of 10,949.
Both YAFS surveys collected information on depressive symptoms using the Center for Epidemiological Studies-Depression (CES-D) Scale, a 20-item measure where the respondents are asked to rate how often they experienced symptoms associated with depression, such as restless sleep, poor appetite, and feeling lonely. The researchers only used 11 items “to enable direct comparison.”
Response options range from 0 to 3 for each item (0 = Rarely or None of the Time, 1 = Some or Little of the Time, 2 = Moderately or Much of the time, 3 = Most or Almost All the Time). Scores range from 0 to 60, with high scores indicating greater depressive symptoms.
Vulnerable groups
The researchers examined the differences in depression scores with respect to respondents’ age, sex, education, marital status and socioeconomic status, place of residence, and sexual orientation, gender identity and expression (Sogie), and educational attainment.
According to the study, the surge of MSDS prevalence was especially notable among the marginalized youth groups of females, members of the LGBT+, those with lower education levels, those from the poorest families, and those who are separated, widowed or divorced from their partners.
MSDS rose the highest among Filipino youth who are noncisgender—from 7 percent in 2013 to 32.3 percent in 2021, or a growth of 25.3 percentage points. Noncisgender is an umbrella term for individuals whose gender identity does not align with the sex they were assigned at birth, including transgender, genderfluid, or nonbinary.
Pandemic impact
This is followed by youth who are separated/widowed/divorced with MSDS prevalence increasing by 23 points from 18.3 percent to 41.3 percent, compared to their married and single counterparts.
The number of Filipino youth with MSDS also climbed the highest among those who were unable to complete elementary education: from 10.8 percent to 26.5 percent (up by 15.7 points); and those belonging in the poorest households: from 10.6 percent to 25.1 percent (up by 14.5 points).
Female youth also grew more depressed compared to their male peers, with MSDS prevalence rising from 10.8 percent to 24.3 percent, up by 13.5 points.
“These disparities indicate that certain populations are more likely to experience depression and face greater barriers to accessing necessary mental health services,” the study said.
The significant increase in the number of Filipino youth with MSDS could be largely attributed to the COVID-19 pandemic, it added.
“The pandemic exposed people and communities to higher levels of stress and crisis while greatly reducing access to support and services,” it said, citing earlier similar studies. “This is especially true for marginalized groups that are more likely to experience social inequalities.”
The Philippines had one of the longest and strictest lockdowns leading to prolonged school closures. This resulted in many students being cut off from essential mental health support from counselors and peer networks.
For youth in low-income households, being forced to switch to online learning—where access to digital tools and quiet learning spaces were often lacking—added to the strain.
The lockdowns also kept Filipinos indoors, reducing opportunities for social interaction and physical exercise, sports and leisure, which are significant factors for wellbeing.
Tech, social media
But it was also likely that depression among Filipino youth was already in the upswing even before the pandemic, as revealed by previous studies.
Among the proposed explanations for this global trend was widespread use of digital technology and social media.
The pandemic also accelerated the adoption of teletherapy as a practical and scalable method of delivering mental health services. However, access to teletherapy among Filipinos is largely limited to those with the financial means, technological resources and private spaces.
Youth-friendly services
The researchers called for expanded access to quality and youth-friendly mental health services, and for the stronger implementation of Republic Act No. 11036, or the Mental Health Act of 2018.
It also urged both the government and the private sector to invest in teletherapy to make it accessible among low-income households, and to develop alternative mental health services based in the community and led or supported by peers.